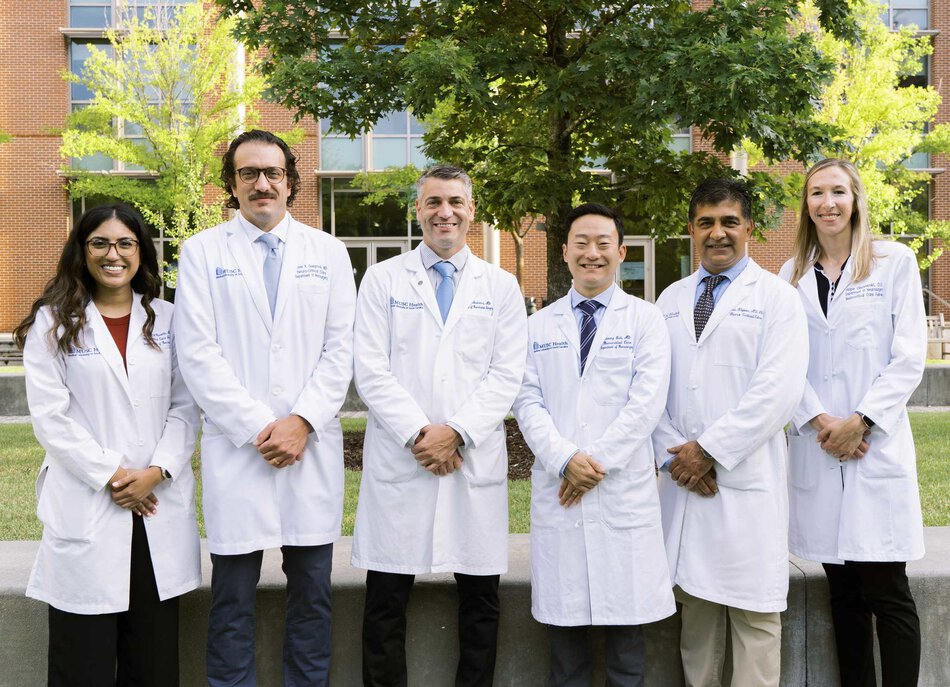
The Neurocritical Care Fellowship at the Medical University of South Carolina (MUSC) is built around a simple principle: do what’s right for the patient, not what’s easy.
We believe that exceptional outcomes come from relentless curiosity, teamwork, and purpose. Our fellows are physicians who bring passion, grit, and compassion to the bedside; and who thrive in an environment where every decision matters.
The Medical University of South Carolina (MUSC), located in historic downtown Charleston, is a vibrant academic medical center and a leading tertiary and quaternary referral hospital for the Lowcountry and beyond. Founded in 1824, MUSC has grown into a 700+ bed institution designated as a Level I trauma center and Joint Commission–certified Comprehensive Stroke Center, offering unmatched exposure to the full spectrum of neurological and neurosurgical emergencies.
Our Neuroscience Intensive Care Unit (NSICU) serves as the hub of the state’s premier neurosciences program, providing advanced care for patients with life-threatening brain and spinal injuries. Through one of the nation’s most extensive telemedicine and telestroke networks, connecting more than 30 hospitals across South Carolina, our team ensures that expert neurocritical care reaches patients wherever they are.
Year over year MUSC treats over 250 aneurysmal SAH patients and performs over 200 mechanical thrombectomies for patients with ischemic stroke. In addition to our ACGME-accredited Neurocritical Care Fellowship, MUSC offers advanced fellowship training in Cerebrovascular Neurology, Neuroendovascular Surgery, and Spine Surgery, reflecting our commitment to comprehensive, multidisciplinary training and excellence in patient care.
Our Unit
The Neurosciences Intensive Care Unit (NSICU) is a state-of-the-art, 23-bed unit located on the 8th floor of MUSC Health University Hospital. It is a closed, fellowship-driven ICU staffed by dedicated neurointensivists, advanced practice providers, and nurses whose expertise and camaraderie define our culture. We own our procedures, we own our decisions, and we own our patients’ outcomes.
The unit is fully equipped for advanced multimodality monitoring, including continuous EEG, ICP/PbO2, and updated bedside ultrasound, bronchoscopes, video laryngoscopy, and invasive / noninvasive hemodynamic monitoring. We collaborate daily with Neurosurgery, Neurology, and Neuroendovascular Surgery, while maintaining primary management of every patient under our care.