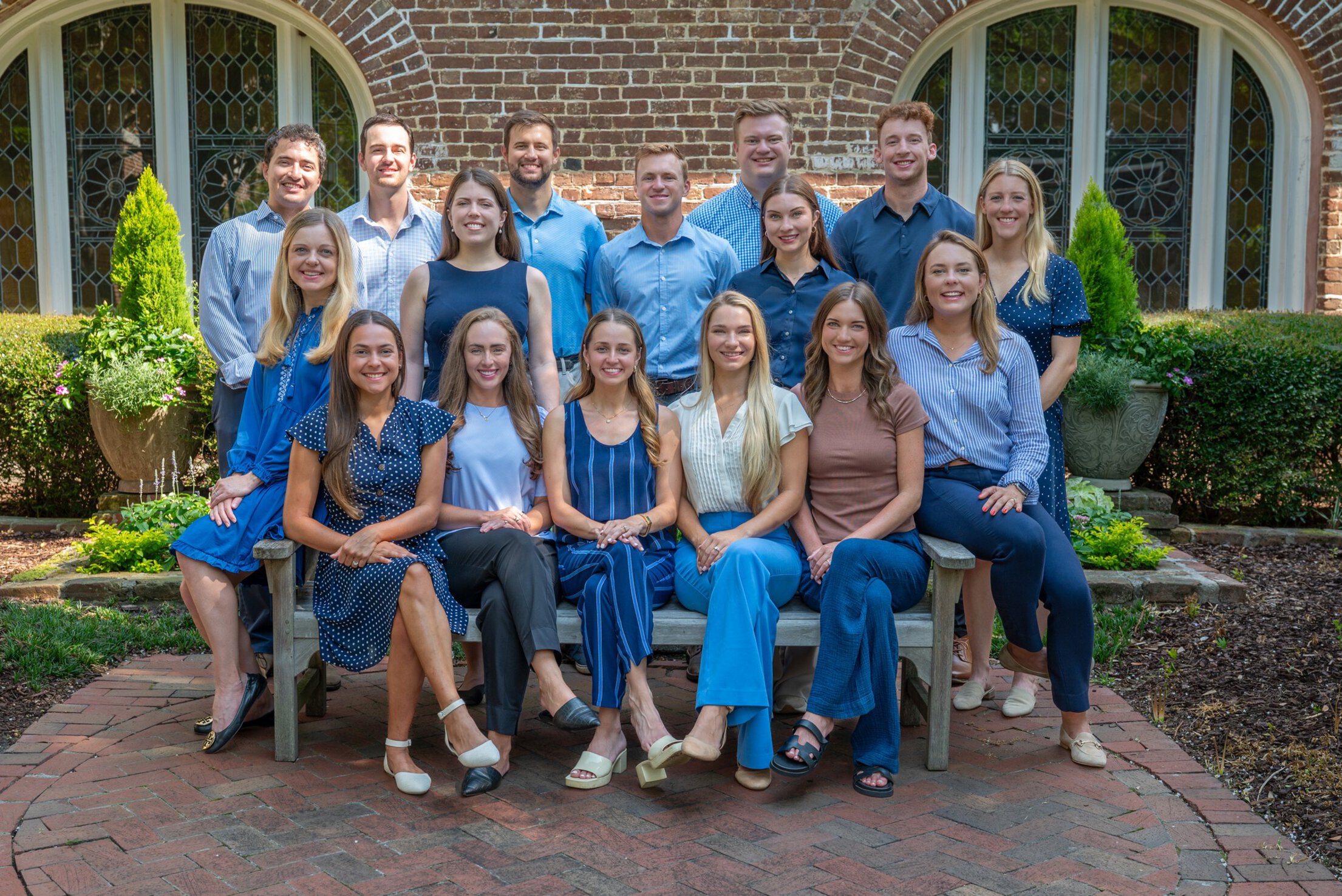
Welcome to MUSC Family Medicine Residency
On behalf of the Medical University of South Carolina (MUSC) Family Medicine Residency Program, I am thrilled to welcome you as you embark on this journey of becoming a Family Medicine physician!
Training at MUSC offers a unique academic institution where the primary care culture is deeply rooted in principles of patient-centered care, innovation, and collaboration, that are celebrated by the Dean of the College of Medicine, Dr. Terry Steyer. As a family physician and former president of Society of Teachers of Family Medicine, Dr. Steyer recognizes primary care as the cornerstone of a thriving healthcare system, where prevention, early intervention, and continuity of care are paramount.
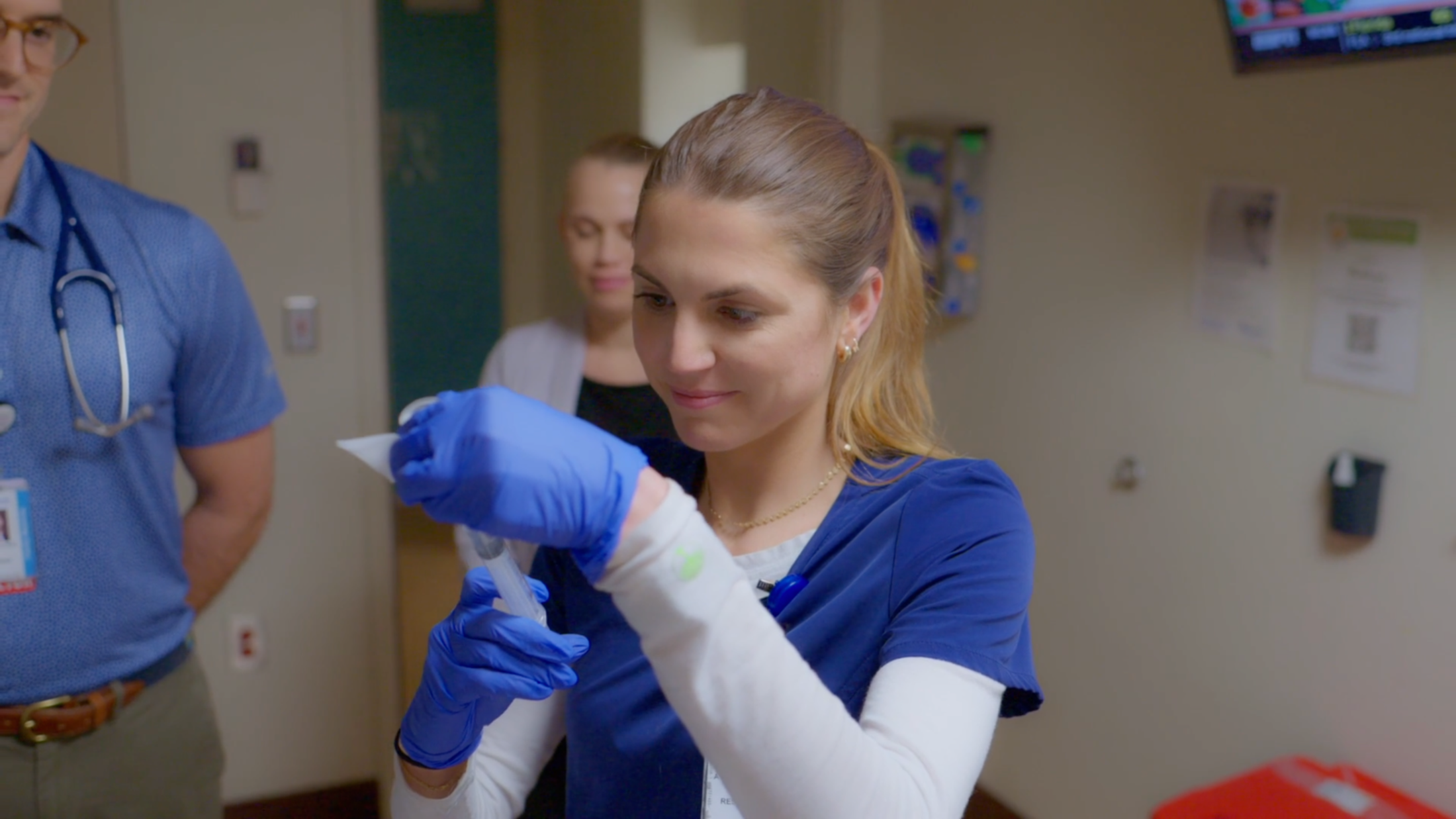
Our curriculum is designed to provide you with a rich and immersive learning experience, blending didactic instruction with hands-on clinical training in a wide variety of settings, including outpatient clinics, community events, and urban hospitals. Whether you're managing chronic conditions, covering a local sporting event, or providing longitudinal care to the elderly in one of our continuing care retirement communities, you'll find ample opportunities to apply your knowledge and skills in real-world scenarios under the guidance of experienced preceptors. Through our patient-centered medical home model, you'll learn to build meaningful relationships with your patients, engage in shared decision-making, and provide personalized care that meets the unique needs of individuals and families across the lifespan.
Moreover, our program is deeply invested in supporting the professional growth and well-being of our residents. Whether you're pursuing research opportunities, participating in community outreach initiatives, or preparing for fellowship application, you'll find a supportive network of colleagues and mentors who are dedicated to helping you succeed in your personal and professional endeavors. We value the breadth of careers a residency training in Family Medicine can result in and are committed to providing high-quality training for residents interested in pursuing everything from certification in integrative medicine, a career in academic medicine, a fellowship in geriatrics or sports medicine, and everything in between!
As you explore your options for residency training, I encourage you to consider the enriching educational experience and vibrant culture of family medicine at MUSC. We are committed to nurturing the next generation of family physicians and empowering them to make a lasting impact on the health and well-being of individuals and communities worldwide.
Once again, welcome to MUSC. We are honored to have you as part of our family medicine community, and we look forward to seeing the incredible contributions you will make to the field of medicine.
Respectfully,